A 70 year old female patient with viral pneumonia secondary to covid 19
June 12th 2021
Bhavani Akula
8th semester
roll.no-150
This is online E log book to discuss our patient’s de - identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE DISCUSSION
CHIEF COMPLIANTS
A70 year old female came to opd on 11/5/2021with chief compliants of
> fever since 5 days
>dry cough since 5 days
>shortness of breath since 3 days
>generalised weakness since 3 days
HISTORY OF PRESENT ILLNESS
Patient was apparantly asymptomatic 5days back
>Then she developped fever since 5 days,which is rapidly progressive
>cough since 5 days,which is dry in nature
>tested (rapid antigen test)-covid 19 positive -3days back
>shortness of breath since 3 days-grade 3
>generalised weakness since 3 days
PAST HISTORY
Known case of- Hypertension since 2 years
>Diabetes mellitus since 2 years
Not a known case of Asthma,TB,Epilepsy
PERSONAL HISTORY
=> DIET - mixed
· => APPETITE- normal
· => SLEEP- Adequate
· => BOWELS- Regular
· => MICTURATION - Normal
· => ADDICTIONS- None
· => ALLERGIES-None
FAMILY HISTORY
There is no significant family history
GENERAL EXAMINATION
The patient was conscious, coherent and cooperative. He is well oriented to time, place and person.
He is moderately built and is moderately nourished.
· > No pallor
· >No icterus
· >No cyanosis
· > No clubbing
· > No generalized lymphadenopathy
· >No pedal oedema
VITALS
VITALS AT THE TIME OF ADMISSION(11/5/2021)
· >Temperature-Febrile
>Pulse-97beats/min
>Blood pressure-120/80mmHg
>Spo2-93% at 16 lit of O2
VITALS ON (11/5/2021) (4.50 PM)
>Temperature-98 F
>Pulse-92beats/min
>Blood pressure-110/60mmHg
>Spo2-99% at 15lit of O2
VITALS ON (12/5/2021) (8AM)
>Temperature-Afebrile
>Pulse-92beats/min
>Blood pressure-130/90mmHg
>Spo2-94% at 15 lit of O2
>GRBS-338mg/dl
VITALS ON (13/5/2021)
>Temperature-98 F
>Pulse-112beats/min
>Blood pressure-120/80mmHg
>Spo2-85% at 16 lit of O2
VITALS ON (13/5/2021) (4.13PM)
>Pulse-57beats/min
>Blood pressure-160/80mmHg
>Respiratory rate-60/min
>Spo2 73% at 16 lit of O2
SYSTEMIC EXAMINATION
=>Cardio vascular system: S1,S2 are heard.No murmurs are heard.
=>Respiratory system:
>Dysppnoea,Wheeze present
>Position of trachea-central
>Breath sounds-vesicular
>Adventitious sounds-Rhonchi
=>Per Abdomen: Soft,Non-tender,No organomegaly
=>CNS Examination: Intact
PROVISIONAL DIAGNOSIS
,
Viral pneumonia secondary to covid-19 with Type2 DM,HTN
TREATEMENT HISTORY (11/5/2021)
1)Head end elevation
2)O2 inhalation to maintain Spo2>90%
3)IVF-NS-With Optineuron 50ml/hr
4)Inj.Dexamethasone 8mg IV/OD
5)Inj.Pantop 40mg IV/OD
6)Inj.Clexane 40mg SC.OD
7)Duolin Budecort/Nebulization 6th hrly
8)Tab.MVT OD
9)Tab.Vit C OD
10)GRBS 4th hourly
11)Temp charting 4th hrly
12)PR,BP,SpO2 monitoring hourly
TREATEMENT HISTORY (12/5/2021)
1)O2 inhalation-Maintain SpO2>92%
2)IVF-NS-cont.infusion with 1 ampule of Optineuron
3)Inj.Dexamethasone-8mg IV/OD
4)Inj.Pantop-40mg/IV/OD
5)Inj.Clexane-40mg/SC/OD
6)Nebulisation with Duolin-6th hrly
7)T.MVT-PO/OD
8)T. Limcee-PO/OD
9)Temp.charting 4th hrly
10)Monitor vitals
11)GRBS 4th hrly
12)Inj.HAI according to slicing scale
13)BP monitoring 4th hrly
14)Tab.Olkem-40
TREATMENT HISTORY (13/5/2021)
1)O2 inhalation maintain SpO2>90%
2)IVF-NS-cont.infusion with 1amp of Optineuron
3)Inj.Dexamethasone 8mg/IV/OD
4)Inj. Pantop 40mg/IV/OD
5)Inj. Clexane 40mg/SC/OD
6) Nebulization with Duolin 6th hrly
7)T. MVT - PO/OD
8)T. Limcee- PO/OD
9)Temp. charting 4th hrly
10)Monitor vitals
11)GRBS monitoring 4th hrly
12)Inj. HAI according to sliding scale
13)BP, PR, SpO2 monitoring
14)T. Omlesartan 40mg OD
S
Syp. Cactulose 15ml
Immediate cause of death- Type 2 Respiratory failure
Antecedent cause of death-Severe covid-19 pneumonia
INVESTIGATIONS
ECG :
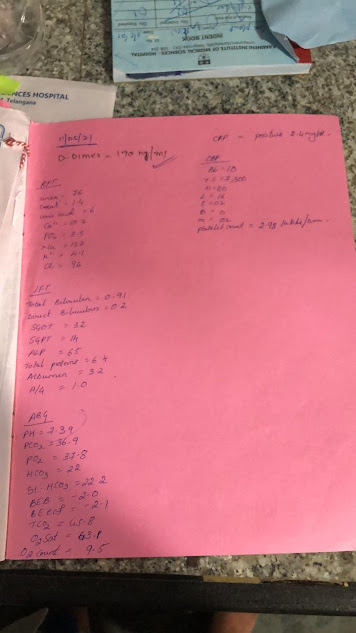
D-dimer, RFT, LFT, ABG, CRP, CBP:
5)
I would like to thank Dr.Rakesh Biswas Sir for giving me this opportunity and
Dr.Kranthi Mam for the guidance
I



Comments
Post a Comment