MEDICINE CASE DISCUSSION
Online blended bimonthly assignment toward summative assessment for the month of May 2021
A.Bhavani
Roll.no 150
8th sem.
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
1) What is the most probable diagnosis in this
1ans)
*Differential diagnosis:
à => Ruptured Liver Abscess.
· =>Organized collection secondary to Hollow viscous Perforation.
· => Organized Intraperitoneal Hematoma.
· => Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
· =>Grade 3 RPD of right Kidney
=>The most probably diagnosis is there is abdominal hemorrhage.
=> This will give reasoning to the abdominal distention, and the blood which is aspirated.
2) What was the cause of her death?
2ans)
=>After leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery.
=>The patient passed away the next day.
=>Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
3ans)
=>NSAID-induced renal dysfunction has a wide spectrum of negative effects, including
decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal
failure.
=> Chronic NSAIDs use has also been related to hepatotoxicity.
=> While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well
known, NSAIDs have also been associated with hepatic side effects ranging from
asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to
fulminant liver failure and death.
5) Nephrology (and Urology) 10 Marks
=>Considering the following factors:
QUESTION 1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
1. 1ans)
=>3 yeaars ago- diagnosed with hypertension
2. =>21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
3. =>18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
4. => 11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
5. =>4 days ago-
> patient presented to casualty in altered state with facial puffiness and periorbital edema and weakness of right upper limb and lower limb
> towards the evening patient periorbital oedema progressed
> serous discharge from the left eye that was blood tinged
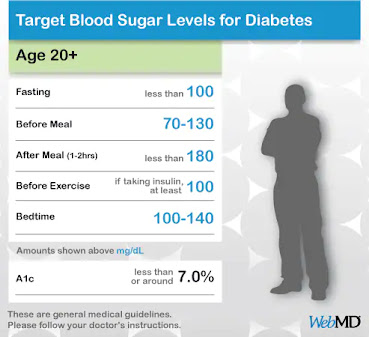
> was diagnosed with diabetes mellitus
6. => patient was referred to a government general hospital
7. => patient died 2 days ago
a =>patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then.
T =>This resulted in poorly controlled
blood sugar levels.
T => The patient was diagnosed with acute oro rhino orbital mucormycosis .
rh => Rino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes
( https://www.cdc.gov/fungal/diseases/mucormycosis/definition.html ) the fungus enters the sinuses from the environment and then the brain.
=>The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA .QUESTION 2: What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?2ans)
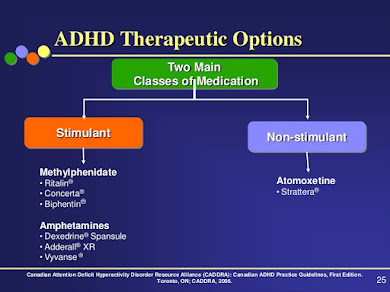
*The proposed management of the patient was
>inj. Liposomal amphotericin B according to creatinine clearanc
> 200mg Iitraconazole was given as it was the only available drug which was adjusted to his creatinine clearance
>Deoxycholate was the required drug which was unavailable
https://pubmed.ncbi.nlm.nih.gov/23729001/ this article talks about the efficacy and toxicity of different formulations of amphotericin B
=>along with the above mentioned treatment for the patient managing others symptoms is also done by-
I. * Management of diabetic ketoacidosis –
=>Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
=>Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood.
= =>Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
=> Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
QUESTION 3: What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
3ans)
=>Mucormycosis is may be being triggered by the use of steroids, a life-saving treatment for severe and critically ill Covid-19 patients.
=>Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus.
=> But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
=>With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing
9) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
link for information about covid-master chart
https://docs.google.com/spreadsheets/d/1OwqoGOD5TVsyQhfpgXNoQCV_CZp5aT18Csxq3hXrurk/edit?usp=sharing
1) Covid 19 with co morbidity (Pulmonology/Rheumatology)
https://nikhilasampathkumar.blogspot.com/2021/05/covid-pneumonia-in-pre-existing-case-of.html
Questions:
1) How does the pre-existing ILD determine the prognosis of this patient?
- The pre-existing ILD significantly worsens the prognosis of this covid patien
- Interstitial lung disease is characterized by dyspnea, decreased pulmonary diffusing capacity, decreased FVC and TLC. The SpO2 of these patients is usually decreased due to increased A-a gradient
- A superimposed covid-19 infection in these cases can cause an acute exacerbation of symptoms such as dyspnea, decreasing levels of SpO2 further and faster than in Covid-19 patients without interstitial lung disease.
- Radiology (HRCT) usually shows the development of new pulmonary opacities and fibrosis.
Patient factors:
- Since this patient already had a reduced SpO2 of 90-92% (compared to the normal range of >96%) she is more susceptible to worsening of hypoxia and dyspnea unless immediate ventilator support is provided
- The patient reportedly did not have dyspnea prior to the covid infection but developed a grade 2 SOB
- ILD by itself makes the patient much more susceptible to acquiring Covid-19 infection.
Prognosis: Poor
Source: https://ejrnm.springeropen.com/articles/10.1186/s43055-021-00431-2
2) Why was she prescribed clexane (enoxaparin)?
- The main pathogenesis of systemic inflammation caused by Covid-19 is by inducing a cytokine storm that causes epithelial cell necrosis, increased vascular permeability, dysfunctional humoral and CMI which all collectively lead to acute lung injury and ARDS
- Of these cytokines, IL-6 is one that is the most important in determining the prognosis. IL-6 levels are highly elevated in patients with severe disease
- Enoxaparin is said to relieve and prevent inflammation produced by IL-6 by inactivating it by binding it with its non-anticoagulant fraction, especially in pulmonary epithelial cells.
- Moreover, patients with Covid-19 are more susceptible to the development of venous thromboembolism, which can be prevented by Enoxaparin (LMWH).
CASE 9-2: COVID-19 SEVERE
https://nehapradeep99.blogspot.com/2021/05/a-50-year-old-female-with-viral.html
QUESTIONS:
1) Since patient didn't show any previous characteristic diabetes signs, did the Covid-19 infection aggravate any underlying condition and cause the indolent diabetes to express itself? If so what could be the biochemical pathways that make it plausible?
The patient may have already had slight hyperglycemia, owing to high HbA1c levels (7.1%), which may have aggravated due to COVID-19. The possible biochemical pathways include: [6]
2) Did the patient's diabetic condition influence the progression of her pneumonia?
=>Yes, with DM or hypergycemia in patients leads to an increase in COVID-19 severity. Also, poor glycaemic control predicts an increased need for medications and hospitalizations, and increased mortality.
=>In monocytes: elevated glucose levels increase SARS-CoV-2 replication, and glycolysis sustains SARS-CoV-2 replication via the production of mitochondrial reactive oxygen species and activation of hypoxia-inducible factor 1α. Therefore, hyperglycaemia supports viral proliferation.
3) What is the role of D Dimer in the monitoring of covid? Does it change management or would be considered overtesting?
=>D- Dimer levels indicate the severity of COVID-19, pertaining to possible thrombotic complications- as D Dimer is formed post- fibrinolysis.
=>D- Dimer does change the management, as D-Dimer levels above 2000ng/dl were found to have a direct link with increasing severity of COVID-19 [7]. Moreover, D- dimer levels would be helpful in fast diagnosis and prevention of thrombotic complications.
CASE 9-3 (COVID-19 SEVERE)
https://143vibhahegde.blogspot.com/2021/05/covid-in-26-yo-female.html
QUESTIONS:
1. Why was this patient given noradrenaline?
Following kidney failure, the patient had sudden and persistent hypotension. To combat this, the patient was given noradrenaline, a potent vasoconstrictor.
2. What is the reason behind testing for LDH levels in this patient?
LDH (Lactate Dehydrogenase) catalyzes the conversion of lactate to pyruvate and back. Hence, an increase in LDH denotes some form of tissue damage. In this patient, an increase in LDH levels would denote inflammation, and a high increase would denote Multi-Organ Failure.
3. What is the reason for switching from BiPAP to mechanical ventilation with intubation in this patient? What advantages did it provide?
Although BiPaP is a positive pressure system, unlike tracheal intubation, it does not send the air to the trachea and depends on the patient's ability to respire. In this patient, as SpO2 levels were dropping to 30% despite BiPAP, a more invasive method was required to push the air directly into the lungs- hence intubation was preferred.
CASE 9-4 (COVID-19 MILD)
https://gsuhithagnaneswar.blogspot.com/2021/05/29-year-old-male-patient-with-viral.html?m=1
QUESTIONS:
1. Is the elevated esr due to covid related inflammation?
Yes, as ESR is an important indicator of immunological loss, and owing to an increased inflammation and immunological dysfunction in COVID, elevated ESR is most likely dur to COVID related inflammation.
2. What was the reason for this patient's admission with mild covid? What are the challenges in home isolation and harms of hospitalization?
Hospitalisation was due to Grade 3 Shortness of Breath (SOB), and long duration of COVID-19 infection.
Challenges of home isolation-
- Physical challenges- Many patients may find it hard to cut themselves from the outside world and confine themselves to a room for long periods of time
- Emotional challenges- Sitting in a small room all day leads to stress, anxiety and even depression, with an increase in mental health issues being reported during the pandemic
- Social challenges- Members of society who cannot care for themselves on their own (eg, patients with disability, geriatric patients etc) are at a major loss
- Economic challenges- Some patients, such as daily wage labourers, cannot afford to home isolate as they need to earn on a daily basis to keep their family going
Harms of hospitalisation-
- Infection- Members visiting may get COVID from exposure to the hospital ward alone
- Cost- PAtient may not be able to bear the brunt of high costs
- Overtesting- Hospitals may ask the patients to stay overnight despite the conditions being mild, based on preliminary test results
- Economic- Working patients may have to take a leave of absence, hence affecting both their work and decreasing their salary, on top of spending money on hospitalisation
CASE 9-5 (COVID-19 SEVERE)
https://anuragreddy72.blogspot.com/2021/05/case-discussion-on-hypokalemic-periodic.html
QUESTIONS:
1) What was the reason for coma in this patient?
The reason for coma is due to severe hypoxia, as his SpO2 levels were 20% when he was admitted. Along with this, hypokalemia leads to respiratory muscle paralysis, which may have aggravated his dyspnoea.
2) What were the competency gaps in hospital 1 Team to manage this intubated comatose patient that he had to be sent to hospital 2? Why and how did hospital 2 make a diagnosis of hypokalemic periodic paralysis? Was the coma related?
The main competency gap was in the lack of testing for serum electrolytes, as the hypokalemia had caused weakness and fatigue in this patient.
Hospital 2 make a diagnosis of hypokalemic periodic paralysis based on the fact that the patient had generalised weakness before becoming comatose, along with tingling and symptoms of paralysis. On testing serum electrolytes, his potassium levels were found to be 2.3 mEq/L (normal-3.5-5)
The coma was most probably related, as hypokalemia can cause respiratory muscle paralysis, leading to aggravation of hypoxia, hence causing unconsciousness in the patient.
3) How may covid 19 cause coma?
Yes, as the brain is extremely sensitive to oxygen, oxygen deprivation due to COVID-19 can lead to a comatose state.
This patient had very low SpO2 levels (20%), which may have caused the coma.
CASE 9-6 (COVID-19 WITH ALTERED SENSORIUM)
https://vijaykumarkasturi.blogspot.com/2021/05/65-years-old-male-with-viral-pneumonia.html
QUESTIONS:
1. What was the cause of his altered sensorium?
Probable causes include
1. Altered sensorium due to hypoxia, leading to hypercapnic encephalopthy and altered sensorium
2. Increased urea levels leading to uraemic encephalopathy, which causes altered sensorium
2. what is the cause of death in this patient?
The cause of death in this patients was due to complications of COVID-19, most probably Acute Kidney Failure (AKI), as denoted by increased urea and creatinine, and hypoproteinemia. Hypoxia and inflammatory response due to COVID-19 may have triggered the process.
Source: https://www.frontiersin.org/articles/10.3389/fphar.2020.579886/full
case-7) A 67 year old lady in the ICU with COVID induced Viral
Pneumonia .
https://drsaranyaroshni.blogspot.com/2021/05/a-67-year-old-lady-in-icu-with-covid.html
Q1. What is the grade of pneumonia in her?
A. Based on the CT severity score it can be said that the patients pneumonia is moderate.
Q2. What is the ideal day to start steroids in a patient with mild elevated serum markers for COVID ?
A. It is best to start the treatment with dexamethasone before the onset of cytokine storm.
Q3. What all could be the factors that led to psychosis in her ?
A. The following can lead to ICU psychosis
- Sensory deprivation
- Sleep deprivation
- Stress
- Continuous light levels
- Continuous monitoring
- Lack of orientation
- pain
- drug reactions
- Infections
- metabolic disorders
- Dehydration
Q4. In what ways shall the two drugs prescribed to her for psychosis help ?
A. Pirecetam improves memory and causes cognitive enhancement and also improves mood.
Resperidone acts by decreasing the dopaminergic and seritonergic pathways in the brain
Q5. What all are the other means to manage such a case of psychosis?
A. The management of ICU psychosis primarily depends on the cause. If it is sleep deprivation then hte patient should be provided a peaceful place to take rest.
If it is due to underlying conditions like heart failure and dehydration then these should first be corrected.
Haloperidol is a medication commonly used to manage ICU psychosis. Other common anti-psychotics can also be used.
A. The patient is supposed to self isolate after they are discharged for another 7 days after discharge. If possible oxygen levels are to be monitored as well for the next 7 days. The patients and the patient's attenders should be on the look out for danger symptoms such as
trouble breathing, chest pain, bluish discolouration of lips, confusion or inability to wake up.
Q7. What are the chances that this patient may go into long covid given that her "D Dimer" didn't come down during discharge?
A. Long COVID is the persistence of symptoms such as cough, breathlessnes, headaches and chest pain weeks to months after discharge. People suffering from long COVID usually have elevated biomarkers such as elevated d dimer and CRP. As this patient has elevated d dimer levels at discharge there is a good chance that she could suffer from long COVID.
case-8) 35YR/M WITH VIRAL PNEUMONIA SECONDARY TO COVID
19 INFECTION
https://bhavaniv.blogspot.com/2021/05/35yrm-with-viral-pneumonia-secondary-to.html?m=1
Q1. Can psoriasis be a risk factor for severe form of COVID?
A. There is no evidence that patients with moderate-to-severe psoriasis receiving systemic treatments, including biologics, have higher risk of SARS-CoV-2 infection and/or increased hospitalization and death related to COVID-19 compared to the general population.
Q2. Can the increased use of immunomodulatory therapies cause further complications in the survivors?
A. Immunomodulators help COVID 19 patients by suppressing the cytokine storm but they also have thepotentialt to increase the risk of infection (like mucormycosis), traditional clinical signs may be masked with resulting delays in identification and treatment.
Q3. Is mechanical ventilation a risk factor for worsened fibroproliferative response in COVID survivors?
A. Increasing evidence from experimental and clinical studies suggests that mechanical ventilation, which is necessary for life support in patients with acute respiratory distress syndrome as seen in COVID 19 can cause lung fibrosis, which may significantly contribute to morbidity and mortality. It is believed that ventilator induced lung injury is the cause for the fibroproliferative changes and the resultant lung fibrosis.
case-9) 45 year old female with viral pneumonia secondary to Covid-19
https://vidya36.blogspot.com/2021/05/comparative-study.html?m=1
Q1. What is the type of DM the patient has developed ?(is it the incidental finding of type 2 DM or virus induced type 1DM)?
A. Incedental type 2 DM can be differentiated from de novo covid induced type 1 DM with the help of the HbAc1 levels.
As HbAc1 levels are indicators of long term blood ssugar levels they are likely to be raised in pre existing DM that was incidentally discovered. But in case ofthe diabetes being de novo in nature then the HbAc1 levels are unlikely to be raised. As the patients HbAc1 levels are not raised we can not at this point determine if the patient has incedental discovered type 2 DM or Covid induced de novo DM.
Q2. Could it be steroid induced Diabetes in this patient?
A. As the patient was given dexamethasone as a part of her treatment regimen it is possible that her elevated glucose levels are a result of steroid induced hyperglycemia.
case-10) A little difference that altered the entire covid recovery
game: a report of two patients with focus on imaging findings.
https://vidya36.blogspot.com/2021/05/comparative-study.html?m=1
Q1. What are the known factors driving early recovery in covid?
A. The following factors can lay a role:
- Younger age ggroup
- shorter duration of fever
- No diabetes
- PaO2/FiO2 levels
- No comorbidities
case-11) Viral pneumonia secondary to COVID of a denovo Diabetes Mellitus
https://rishithareddy30.blogspot.com/2021/05/covid-case-report.html
1. How is the diabetes related to the prognosis of COVID patients? What are the factors precipitating diabetes in a patient developing both covid as well as Diabetes for the first time?
A. People suffering from diabetes are like to experience more severe symptoms of the disease than the ones who are not diabetic. Even within the patients that are diabetic the people whose disease is under better control tendtendvbe better diagnosis.
Possible causes for de nov diabetes in COVID19 include:
· The SARS CoV 2 virus enters the cells through the ACE 2 receptors which are present in large numbers in the pancreas and that this damages the pancreatic cells.
· Another theory is that the inflammation caused by the cytokine storm damages the beta cells.
Q2. Why couldn't the treating team start her on oral hypoglycemics earlier?
A. As the insulin is faster acting as compared to oral hypoglycemics and as her blood glucose level was very high it is important to bring it down as fast as possible.
case-12) Moderate to severe covid with prolonged hospital stay:
https://93deepanandikonda.blogspot.com/2021/05/42-years-female-patient-with-viral.html
Questions:-
1) What are the potential bio clinical markers in this patient that may have predicted the prolonged course of her illness?
Serum LDH: 571U/L (Normal range=140-280U/L
ALP : 342 U/L (Normal range=44-147U/L)
SpO2: 82% at RA (Normal range= >96%)
HR: 124bpm (Normal range=60-100bpm)
Classically, the bio clinical markers that are predictive of a Covid-19 patient's outcome are
- C reactive protein [>57.9mg/dL]
- D-Dimer [>1mcg/ml associated with poorer prognosis]
- Serum LDH [>248U/L]
- IL-6 [2.9 times higher in severe disease compared to mild disease]
- SGPT [Isolated rise in SGPT >3 times the normal value]
- ESR [high sustained level after recovery from infection]
- Albumin
- Platelet count
- Neutrophil count
- NLR: [>5.5]
- Urea
- Creatinine
- High sensitivity Troponin
The patient in question has elevated levels of serum LDH and ALP. Her CRP and D-Dimer levels are not high enough to be considered as a bad prognostic factor.
Sources: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219356/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7194951/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7896696/
case-13) Severe covid with first diabetes
Link to Case report log :
https://vignatha45.blogspot.com/2021/05/58-years-female-patient-with-viral.html
1) What are the consequences of uncontrolled hyperglycemia in covid patients?
- Hyperglycemia can lead to anomalous glycosylation of tissue receptors throughout the body. One of these receptors happens to be ACE2, the same receptor SARS-CoV2 uses to gain entry into the host cell. In fact, glycosylation of ACE2 is necessary for the virus to establish an infection.
- Uncontrolled hyperglycemia freely facilitates this glycosylation, making these patients more susceptible to Covid-19 infections and increasing the severity of the infection by helping increase the viral load (by increasing the concentration of glycosylated ACE2)
- Control of blood sugar can also decrease the chances of a cytokine storm during the second phase of the infection.
- Uncontrolled hyperglycemia hence, suggests a poor prognosis in Covid-19 patients.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7188620/#:~:text=Therefore%2C%20high%20and%20aberrantly%20glycosylated,and%20a%20higher%20disease%20severity.
2) Does the significant rise in LDH suggests multiple organ failure?
Lactate dehydrogenase has 5 isoenzymes that are present in various tissues such as the heart, RBCs, lungs, liver, kidney, brain, and skeletal muscle.
Since covid-19 primarily causes lung damage, LDH3 is released into the blood giving an elevated titer.
Multi-organ damage that involves the heart (myocarditis) or kidneys (renal failure) can lead to an elevation in respected isoenzymes found in these tissues.
Hence, a significant rise in LDH indicates a poor prognosis and points towards multi-organ damage
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7251362/
3) What is the cause of death in this case?
This patient was diagnosed with uncontrolled hyperglycemia with severe covid pneumonia
LFT shows elevated AST, ALT, and ALP with a gross increase in bilirubin titer.
The D-Dimer is elevated (560ng/ml) and the LDH is 835U/L both of which are indicators of a poor prognosis.
The most likely cause of death in this patient seems to be ARDS
The immediate cause of death: Most probably cardio-pulmonary arres
Antecedent cause: Severe covid-19 pneumonia
case-14) Long covid with sleep deprivation and ICU psychosis
https://jahnavichatla.blogspot.com/2021/05/covid-case-discussion.html
Questions:
1)Which subtype of ICU psychosis did the patient land into according to his symptoms?
Hyperactive delirium: Manifests as agitation, restlessness, refusal to cooperate with caregivers, unprovoked mood changes, hallucinations
2)What are the risk factors in the patient that has driven this case more towards ICU psychosis
.Hypertensio
.History of cerebrovascular accident (makes him more prone to a new one
.Steroid use
.Sedative use (Gabapentin)
.COPD
3)The patient is sleep-deprived during his hospital stay. Which do you think might be the most probable condition?
A) Sleep deprivation causing ICU psychosis
B) ICU psychosis causing sleep deprivation is more likely in this patient
4) What are the drivers toward current persistent hypoxia and long covid in this patient?
Elevated bio clinical markers like D-Dimer, LDH, Neutrophils, WBCs(absolute), IL-6, and CRP all contribute to persistent hypoxia and worsen the prognosis. In addition to this, ICU psychosis adds to the prolonged hospital stay.
case-15) Moderate Covid with comorbidity (Truncal obesity and recent hyperglycemia)
https://meghanaraomuddada.blogspot.com/2021/05/case-1-2021-42yr-old-male-with-fever.html
Questions:
1. As the patient is a non-diabetic, can the use of steroids cause a transient rise in blood glucose?
Cortisol stimulates gluconeogenesis in the liver and inhibits glycogen synthesis, increasing blood glucose. Continuous treatment with corticosteroids can lead to elevated blood glucose titers even in non-diabetics.
2. If yes, can this transient rise lead to long-term complications of New-onset diabetes mellitus?
It is still unclear if the alterations brought about by covid-19 in the glucose metabolism are permanent and persist or remit after the resolution of infection. There are ongoing studies that aim to answer these questions
Steroid diabetes is a term coined to describe diabetes mellitus arising as a result of glucocorticoid use for more than 50 years
3. How can this adversely affect the prognosis of the patient?
Hyperglycemia in general is indicative of a poorer prognosis in a patient compared to covid patients with normal blood glucose levels.
4. How can this transient hyperglycemia be treated to avoid complications and a bad prognosis?
Oral hypoglycemics (such as sulfonylureas) are efficient at controlling blood glucose levels in non-diabetics who develop steroid-induced hyperglycemia. Most cases revert to normoglycemia after discontinuation of steroids.
5. What is thrombophlebitis fever?
Fever in response to thrombophlebitis that is caused due to release of inflammatory mediators
6. Should the infusion be stopped in order to control the infusion thrombophlebitis? What are the alternatives?
No, infusion thrombophlebitis is not grounds for discontinuation of infusions that are essential for the treatment of the case. Thrombophlebitis can be treated by local compressive dressings, NSAIDs (topical and/or systemic)
case-16) Mild to moderate covid with hyperglycemia
https://vaishnavimaguluri138.blogspot.com/2021/05/viral-pneumonia-secondary-to-covid-19.html
Questions:
1. What could be the possible factors implicated in elevated glycated HB ( HBA1c ) levels in a previously Non-Diabetic covid patient?
The possible factors that could have led to precipitation of diabetes in a covid-19 patient are
.Genetic susceptibility to diabete
.Pre diabetic state
.Viral insult to the beta cells of the pancreas
.Stress hyperglycemia due to inflammation-induced insulin resistance
.High dose steroid usage
case-17) Covid 19 with hypertension comorbidity
https://prathyushamulukala666.blogspot.com/2021/05/a-62-year-old-male-patient-with-fever.html
1)Does hypertension have any effect to do with the severity of the covid infection.If it is, Then how?
Yes, hypertensive patients are at a higher risk of COVID 19 severity. It is already known that hypertension is assocatied with a weaker immune system and is seen in older patients which show bad prognosis when dealing with this infection. As there is a high risk of developing cardiovascular events as well as end organ failure.
2)what is the cause for pleural effusion to occur??
Pneumonia caused due to COVID-19 infection lead to increase permeability of microvascular circulation which lead to pleural effusion(exudative type)
case-18) Covid 19 with mild hypoalbuminemia
https://meesumabbas82.blogspot.com/2021/05/a-38-yo-male-with-viral-pneumonia.html
QUESTIONS:
1. What is the reason for hypoalbuminemia in the patient?
The reason for hypoalbuminemia in COVID_9 patient is due to increased catabolism of albumin to make amino acids as well as simulataneous decrease in albumin synthesis( albumin is a negative acute phase reactant that means its level decrease during inflammation)
2. What could be the reason for exanthem on arms? Could it be due to covid-19 infection ?
Exanthem is an eruptive skin rash seen in viral infections. Yes, this could be due to COVID-19 infection. The exanthem in COVID-19 resembles that of varicella.
2. What is the reason for Cardiomegaly?
High blood pressure might be the underlying cause for cardiomegaly in this patient.
Uncontrolled high blood pressure leads to increase in work load of the heart. To compensate this demand, the ventricles undergo remodelling leading to cardiomegaly.
3. What other differential diagnoses could be drawn if the patient tested negative for covid infection?
. Chicken pox
.Shingles
. Pytrias
4. Why is there elevated D-Dimer in covid infection? What other conditions show D-dimer elevation?
D-dimer is increased in a COVID-19 patient. It may be related to the viral life cycle. The apoptotic processes target the endothelial cells of the vasculature resulting in triggered coagulopathy and ultimately result in increased d-dimer levels.












































Comments